“Fertility is not just a female issue. It’s a man’s too. I ordered for my husband.”
The Science…
(scroll for reference list and more lifestyle changes)
Hang Out While Hangin' In...
Men, your testicles hang outside your body for a reason. They need to maintain a 2°C cooler temperature in comparison to the rest of your body in order to properly function- make sperm, testosterone, and other hormones. That’s why they sag away from your body when hot and shrivel up when cold. The scrotum also has a higher concentration of sweat glands to regulate temperature. Studies have proven a constricted environment causing compressive heat can lower sperm count to nearly zero, and cause the few remaining sperm to have low motility (they can’t make it through the vaginal canal), and sperm morphology, which is a decrease in sperm quality and abnormal changes in your DNA and gene expression which you pass to your offspring.
Healthy Sperm Leads to Healthy Pregnancy and Healthy Children…
Men with poor-quality sperm, and high levels of sperm DNA fragmentation, have been shown to double the likelihood of a miscarriage occurring. Sperm DNA damage has been linked to numerous diseases and disorders of the offspring including autism, epilepsy, and childhood cancer (Ji et al., 1997; Aitken and Krausz, 2001; Sipos et al., 2004; Vestergaard et al., 2005; Reichenberg et al., 2006) Older fathers have to consider healthy sperm production a top priority as they are much more likely to have sperm morphology. Studies out of Columbia University prove that older fathers are much more likely to face miscarriages, pre-term births, and genetic conditions like schizophrenia, bipolar disorder, and autism spectrum disorder. Doctors are finding that unlike chromosomal abnormalities (down syndrome) which occur more often as a woman ages and can be detected by prenatal tests, glitches in aging sperm are more subtle and are much harder to detect. Men, you have to realize that the health of your sperm, the health of your partner’s pregnancy, and the health of your child, are dependent on a healthy testicular environment and healthy sperm production. Unhealthy sperm leads not just to infertility, but to unhealthy pregnancies that will forever change your life and your family’s life.
Are We Half the Man Our Grandfathers Were? What Changed?
Yes, on average, men today have half the sperm of their grandfathers. Sperm concentration, or the number of sperm per milliliter of semen, has dropped more than 50% among men in Western countries in just under 40 years. Some say that sperm counts are dropping by 1-2 percent per year.
While different environmental and lifestyle choices can lead to infertility we have to ask ourselves what are the major differences between this generation and our grandfathers’ who were 50% more fertile than us with 40% more testosterone. The major environmental change that has affected infertility rates is the increase in toxins such as microplastics and chemicals in our air, water, food, and health-and-beauty products. Living clean and using all-natural products is a must. How about lifestyle? Smoking and heavy drinking can lead to infertility but both have decreased significantly. But sitting and lack of physical movement have drastically increased at rates never before seen. Unfortunately, trends show we don’t seem to be getting up any time soon and our balls are feeling it.
Men’s testicles are meant to hang away from the body to cool themselves down. That’s why they evolved so specifically in the way in which they did. This was essential to our survival as a species. The recent shift from a physically demanding life to one with few physical challenges has been sudden, occurring during a tiny fraction of human existence. The statistics are shocking. American adults sit more than any other time in the history of humanity. Sedentary jobs have increased 83% since 1950 according to the American Heart Association. John Hopkins contends that, “Physically active jobs now make up less than 20% of the U.S. workforce, down from roughly half of jobs in 1960.” In recent decades, affluent populations have become increasingly sedentary, with many adults spending more than 70% of their waking hours sitting. The normal office worker sits a staggering 15 hours every single day. People who have long commutes, even more. And what do most men do when they come home from a long day of sitting at the office and sitting when driving? They sit in front of the TV for another 4 hours on average. No time in our history has man been sitting, overheating, and crushing their packages and we wonder why this fragile testicular sack which has evolved outside our bodies is feeling the effects. Men need to start wearing GP, using the cooling therapy, and getting up a bit more to walk around. Otherwise, we will continue to watch our fertility wither away into the abyss.
Owen N, Sparling PB, Healy GN, Dunstan DW, Matthews CE. Sedentary behavior: emerging evidence for a new health risk. Mayo Clin Proc. 2010 Dec;85(12):1138-41. doi: 10.4065/mcp.2010.0444. PMID: 21123641; PMCID: PMC2996155.
Pizzorno J. Environmental Toxins and Infertility. Integr Med (Encinitas). 2018 Apr;17(2):8-11. PMID: 30962779; PMCID: PMC6396757.
Roberts, N, Americans Sit More Than Anytime In History And It's Literally Killing Us, I write about global public health, behavioral science & innovation, Forbes, Mar 6, 2019
Zhang Y, Guo X, Saitz R, Levy D, Sartini E, Niu J, Ellison RC. Secular trends in alcohol consumption over 50 years: the Framingham Study. Am J Med. 2008 Aug;121(8):695-701. doi: 10.1016/j.amjmed.2008.03.013. PMID: 18691483; PMCID: PMC2562028.
Owen N, Healy GN, Matthews CE, Dunstan DW. Too much sitting: the population health science of sedentary behavior. Exerc Sport Sci Rev. 2010 Jul;38(3):105-13. doi: 10.1097/JES.0b013e3181e373a2. PMID: 20577058; PMCID: PMC3404815.
Commercial Drivers Have Abnormally Low Sperm Counts, Motility, and Quality resulting in Huge Implications for All Men who are Seated and Overheated During the Work Day…
Studies have continued to prove commercial drivers, whether they're truck drivers, taxis, uber, etc. have significantly lower sperm counts, motility, and morphology. One study showed taxi drivers have almost 20% lower prevalence of normal sperm forms. Remember that's abnormal changes in your DNA passed to your offspring resulting in disease, disorder, and miscarriage. Men who could conceive exhibited a longer time to pregnancy. Another study showed just how fast and drastic scrotal temperatures elevated once driving. During the first 20 min of driving, there was a rapid increase from 34.2°C to 35.5°C; from 20 minutes to 120 min of driving, the increase was less rapid, from 35.5°C to 36.2°C. Remember functional scrotal temperature is between 32-35°C. Anything beyond that is not only killing your sperm and changing its DNA but impacting your testosterone and overall health as a man. In this sitting position, testicles are trapped between the thighs, garments, and seat and unable to extend away from the body and sweat as properly needed to regulate temperature. These studies have huge implications for many men who spend hours in the same position but in front of computers, at their desks, at work, or at home. The testicles were specifically designed over millions of years. It couldn’t be more obvious. Until we respect their design, poor testicular environments will have enormous negative effects on male fertility.
Figà-Talamanca I, Cini C, Varricchio GC, Dondero F, Gandini L, Lenzi A, Lombardo F, Angelucci L, Di Grezia R, Patacchioli FR. Effects of prolonged autovehicle driving on male reproduction function: a study among taxi drivers. Am J Ind Med. 1996 Dec;30(6):750-8. doi: 10.1002/(SICI)1097-0274(199612)30:6<750::AID-AJIM12>3.0.CO;2-1. PMID: 8914722.
Louis Bujan, Myriam Daudin, Jean-Paul Charlet, Patrick Thonneau, Roger Mieusset, Increase in scrotal temperature in car drivers, Human Reproduction, Volume 15, Issue 6, 1 June 2000, Pages 1355–1357, https://doi.org/10.1093/humrep/15.6.1355
Male Fertility is a Women’s Health Issue…
Although men are responsible for half of all infertility, a quarter of men are still not tested or treated during an infertility examination. Also, studies suggest around 1 in 5 couples who go through IVF later conceive naturally, which means the lack of male treatment likely leads to overtreatment for women. Women carry most of the treatment burden even when the man has a low sperm count, reduced motility, or abnormal sperm morphology. This must change. We need to bring awareness to these facts as women are serving as treatment surrogates for men, and until that changes, male fertility is a women’s health issue. In most cases, if men were aware of the statistics and the growing male fertility crisis, they would be more than willing to do their share of testing and treatment. Male infertility is usually much easier to solve and affordable than the emotional, expensive, and physically painful experience for women. Sperm rehabilitation is as easy as wearing GP and using GP cooling therapy, change of diet, exercise, and quitting bad habits when trying to conceive such as smoking cigarettes, weed, and excessive drinking. The fastest way to a healthy pregnancy is if both partners take their fertility health seriously.
(Turner KA, Rambhatla A, Schon S, Agarwal A, Krawetz SA, Dupree JM, Avidor-Reiss T. Male Infertility is a Women's Health Issue-Research and Clinical Evaluation of Male Infertility Is Needed. Cells. 2020 Apr 16;9(4):990. doi: 10.3390/cells9040990. PMID: 32316195; PMCID: PMC7226946.)
(Schrock, Leslie. “Male fertility startup state of the union, Market map, deep dive, and where things are going next.”Fertility Rules. 21 Feb 2024.)
(Christopher L R Barratt, Christopher J De Jonge, Richard A Anderson, Michael L Eisenberg, Nicolás Garrido, Satu Rautakallio Hokkanen, Csilla Krausz, Sarah Kimmins, Moira K O’Bryan, Allan A Pacey, Frank Tüttelmann, Joris A Veltman, A global approach to addressing the policy, research and social challenges of male reproductive health, Human Reproduction Open, Volume 2021, Issue 1, 2021, hoab009)
(Thwaites, Jennifer Hall, Geraldine Barrett, Judith Stephenson, How common is natural conception in women who have had a livebirth via assisted reproductive technology? Systematic review and meta-analysis, Human Reproduction, Volume 38, Issue 8, August 2023, Pages 1590–1600)
“We wanted to take every precaution for a healthy pregnancy.”
Testicular Cooling Studies Prove Cooling Therapy Works…
Among the studies published in the Journal of Urology, Dr. Mulcahy showed that sperm density and motility doubled in 65% of his patients after applying ice packs to the scrotal area at night. Dr. Jung discovered in his studies similar significant increases in sperm count and concentration as a result of nocturnal scrotal cooling. Dr. Lavern proved that men who slept and worked in cooler scrotal conditions showed much higher levels of motility compared to men working and sleeping in warmer scrotal conditions. There are even studies proving that sperm is much stronger in the colder months of winter compared to summer as scrotal overheating is more likely in the warmer months. But it is important to note that men must be cautious not to overheat their groins in winter with heated car seats, electric blankets, hot tubs, etc.
The most recent impartial study by doctors Benidir, Remondini, and Jarvi concluded that testicular cooling devices work but men don’t like to wear them as they considered the current devices on the market (before GP launch) as uncomfortable, not discreet, a hindrance on their privacy, not work-friendly, and rapidly losing optimal cooling. They concluded that further innovation is needed for men to use this affordable and natural solution. That's where GP innovation came from, comfort and ease of use first. Our competitors missed another crucial aspect, they don’t solve the major problem of a poor testicular environment.
Mulcahy JJ, ‘Scrotal hypothermia and the infertile man.’ Journal of Urology, 132/3 (1984), pp. 469-70
Jung, A., Schill, W. -B., Schuppe, H. -C., ‘Improvement of semen quality by nocturnal scrotal cooling in oligozoospermic men with a history of testicular maldescent.’ International Journal of Andrology, vol. 28/2 (2005), pp. 93-98
Laven, J. S., Haverkorn, M. J., Bots, R.S., ‘Influence of occupation and living habits on semen quality in men (scrotal insulation and semen quality).’ Eur. J Obstet Gynecol Reprod Biol., vol. 29/2 (1988), pp. 137-41
Malathi A, Iyer RP, Mohan R, Balakrishnan S. Impact of Seasonal Variations on Semen Parameters: A Retrospective Analysis of Data from Subjects Attending a Tertiary Care Fertility Centre. J Hum Reprod Sci. 2023 Apr-Jun;16(2):114-120. doi: 10.4103/jhrs.jhrs_20_23. Epub 2023 Jun 30. PMID: 37547085; PMCID: PMC10404019.
Benidir T, Remondini T, Lau S, Jarvi KA. Evaluation of patient compliance with the use of scrotal cooling devices. F S Rep. 2021 Jun 30;2(3):289-295. doi: 10.1016/j.xfre.2021.06.007. PMID: 34553153; PMCID: PMC8441567.
Overall Male Health...
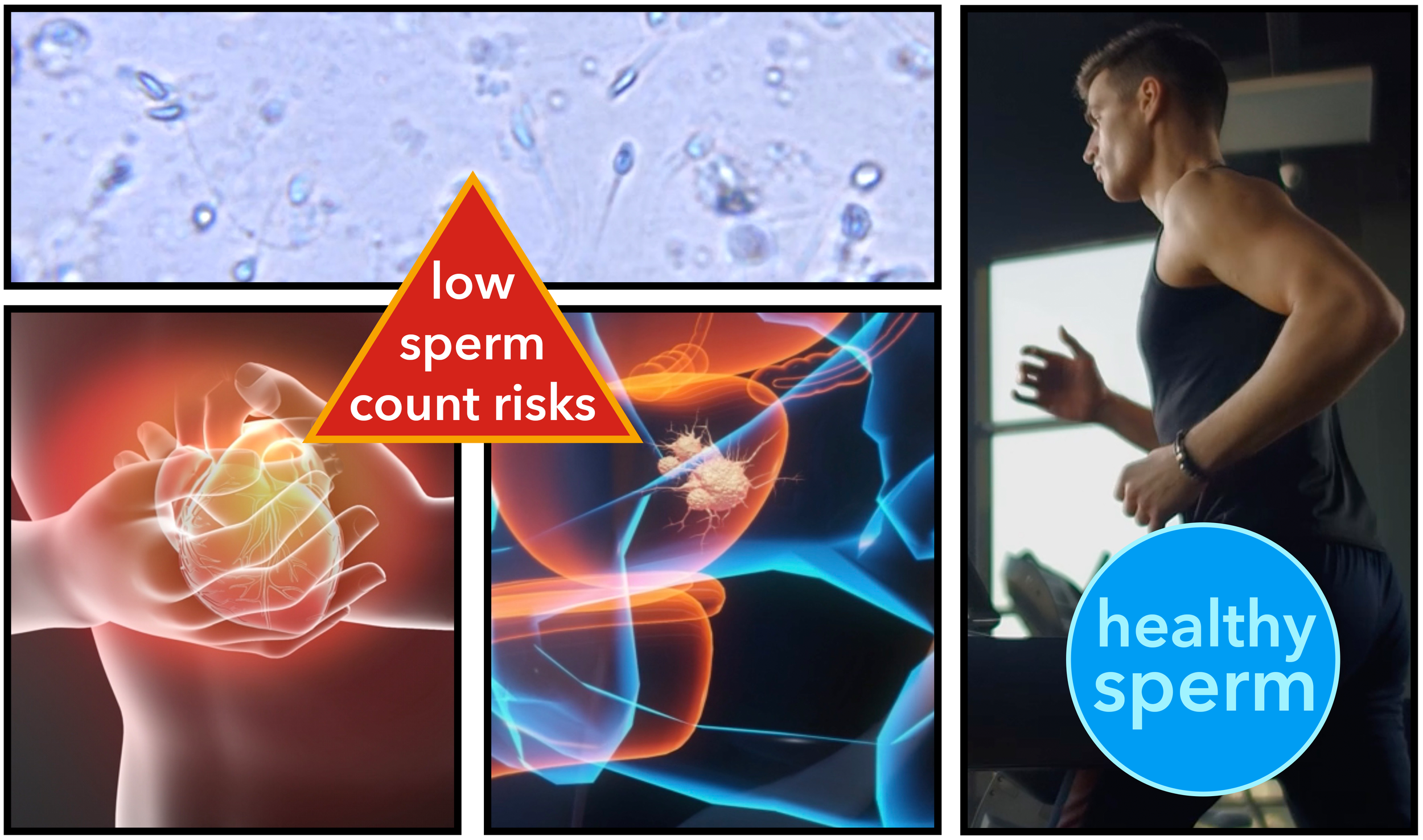
The proper functioning and health of a man’s testicles is directly related to his overall health. Low sperm quality is a direct biomarker for the potential risk of cardiovascular disease, cancer, diabetes, and even longevity of life. The more medical research uncovers the more we discover just how connected our testicular health is to our overall health. So much so that it may become the new norm to have sperm tested not just for fertility reasons but for health reasons. An unhealthy testicular environment also leads to hormonal imbalance. More than 95% of testosterone, the primary stimulus for sperm production, is made in the testes. Testosterone maintains your libido, muscle strength, muscle mass, bone density, fat distribution, and the production of red blood cells and sperm. These functions are what make you a virile and healthy man.
Mental Health…
Large, new studies, including the TemPredict Study, have identified links between depressive symptoms and elevated body temperature. Researchers from UCSF analyzed data from 20,880 individuals collected over seven months, confirming that those with depression tend to have higher body temperatures. “For now, we know that depression is a complex and multi-faceted condition, most likely with many triggers, and body temperature could be playing a role. Given the climbing rates of depression in the United States, we’re excited by the possibilities of a new avenue for treatment,” says psychiatrist Ashley Mason. (There’s a Curious Link Between Depression And Body Temperature, Large Study Finds, Health, 07 February 2024 by David Nield)
Sadly, a new report coming out of the Royal College states that 93% of men dealing with infertility report a deterioration of their mental well-being. This makes sense to most guys who might feel less of a man or heartbroken their dreams of fatherhood might be compromised, as well as, supporting a partner who is devated. The emotional turmoil is heavy and with GP we hope to help as many families as possible through this period, not only with our products but our advocacy.
“At work, I was constantly readjusting and uncomfortable, so happy to solve the problem.”
The Proof is in the Pudding...
Tracking the progress of your sperm count and quality is much easier, more convenient, and more economical than in the past. Now in the comfort of your home, you can test your sperm count and quality using simple at-home sperm tests including- Legacy For Tomorrow Kit, LabCorp Men’s Rapid Fertility Test, Fellow Semen Analysis, MyLAB Box at Home Male Fertility Test, Proov hers and His Fertility Starter Kit, Bird & Be At-Home Sperm Test, and Sperm Check among others. Or you can go the traditional route with your doctor. If after a year of unprotected sex, you still haven't conceived checking your sperm count and quality, as well as, consulting your urologist or fertility specialists is recommended. But the first step is to get ahead of the game with Gentlemen's Parcel. Optimize your sperm count and quality for faster, healthier conception.
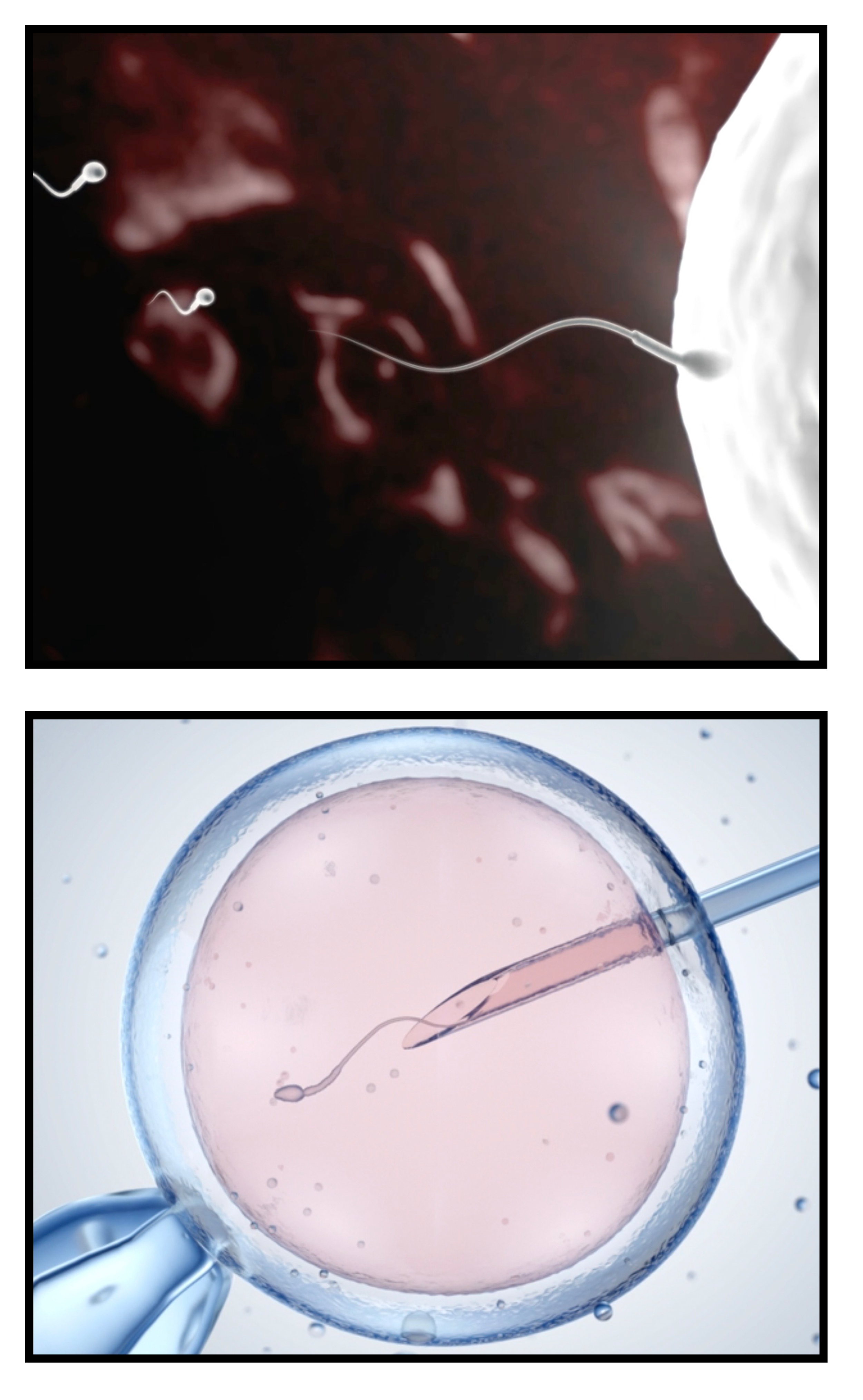
Conceive Naturally or through IVF...
In general men’s sperm count and quality decline after age 35. The idea that men don’t have a biological clock is completely false. In recent decades we have witnessed a pandemic of men of all ages with low testosterone, sperm count, sperm quality, and the inability to conceive naturally. While couples hope to conceive naturally and avoid the emotional turmoil and tens of thousands of dollars associated with treatment, IVF is an incredible gift for couples who cannot conceive. But it is very important to note, that among all the technology, sperm quality is one of the most critical factors for a successful IVF pregnancy. It is imperative to produce the healthiest sperm possible for IVF therapy. Selection is based on motility (ability to move), normal head shape, and overall appearance. The minimal criteria of sperm quality for insemination and IVF therapy includes at least 10 x 10(6) spermatozoa/ml, of which at least 30% are motile and 15% have progressive motility. As a minimum, 20% of spermatozoa should be of normal morphology. Don’t make the mistake of thinking if my sperm isn’t strong enough for natural pregnancy then we can get IVF. No, your sperm has to be healthy enough for IVF too, so please prioritize a healthy testicular environment for healthy sperm production. (Zhao C, Sun L, Zhao P. Effects of sperm processing techniques on IVF pregnancy rates: a mini-review. Ther Adv Reprod Health. 2023 Jul 23;17:26334941231188656. doi: 10.1177/26334941231188656. PMID: 37497119; PMCID: PMC10366343.)
“Even though we can’t conceive naturally, I still want the best specimen for IVF.”
Consult Your Doctor...
Infertility is a complex science and can vary from patient to patient. We recommend consulting your doctor, urologist, or fertility specialist as to the right treatments for you and your family. At the very least Gentlemen's Parcel can be considered an added supplement to your health and fertility goals. But for many cooling therapy was much more than a supplement. After trying all other measures, cooling therapy is what reversed their infertility. Why not start from the beginning with space, air, and cooling therapy to optimize your chances and avoid a difficult and emotional path? Gentlemen's Parcel + a healthy diet and exercise should be your first go-to when thinking to start a family.
Testicular Health is Very Important…
Guys, our testicular environment has a direct impact, positive or negative, not just on your health but on your entire family, including your partner's pregnancy and future children. Some stats include… on average, 15% of men experience infertility. The global prevalence of testosterone deficiency (TD) ranges from 10–40% significantly increasing over the age of 45. 15%-20% of all adult men have varicocele, swollen veins in the scrotum leading to impaired blood flow and temperature regulation in the testicles, a common cause of male infertility and other problems. 1 of every 250 males will develop testicular cancer at some point during their lifetime. Most common testicular conditions include… epididymitis, hydrocele, testicular torsion, varicocele, testicular cancer, spermatocele, orchitis, hernia, kidney stones, hypogonadism, scrotal masses, undescended testicles, testicular injury, pain and swelling. Men with low sperm counts are more likely than those with normal sperm counts to have greater body fat, higher blood pressure, higher “bad” (low-density lipoprotein) cholesterol and triglycerides, and lower “good” (high-density lipoprotein) cholesterol. They also have a higher frequency of metabolic syndrome, and insulin resistance, a condition that can lead to diabetes. Men with low sperm counts had a 12-fold increased risk of hypogonadism or low testosterone levels, and half of them had osteoporosis or low bone mass. Fertility evaluation gives men the unique opportunity for health assessment and disease prevention. Don’t take your testicular health for granted. Get regular check-ups and optimize your healthy testicular environment with Gentlemen’s Parcel.
(Anaissie J, DeLay KJ, Wang W, Hatzichristodoulou G, Hellstrom WJ. Testosterone deficiency in adults and corresponding treatment patterns across the globe. Transl Androl Urol. 2017 Apr;6(2):183-191. doi: 10.21037/tau.2016.11.16. PMID: 28540225; PMCID: PMC5422691.)
(Ferlin, A., Garolla, A., Ghezzi, M., Selice, R., Palego, P., Caretta, N., Di Mambro, A., Valente, U., De Rocco Ponce, M., Dipresa, S., Sartori, L., Plebani, M., & Foresta, C. (2021). Sperm Count and Hypogonadism as Markers of General Male Health. European Urology Focus, 7(1), 205-213. https://doi.org/10.1016/j.euf.2019.08.001)
Post-Vasectomy Healing...
Now if you already have kids or know for sure that you don’t want any then planning a vasectomy may be in your future. A vasectomy is a very low-risk, outpatient procedure. It is much easier, cheaper, and less risky than female sterilization. In the United States, 500,000 men will be getting a vasectomy each year and millions more globally. Rather than the frozen bag of peas, which top urologists still recommend for cooling testicles post-surgery, opt for Gentlemen's Parcel. GP Cooling Therapy is the best product to support post-vasectomy healing as it provides full cooling coverage and the necessary scrotal support recommended by urologists post-surgery.
“My vasectomy doctor literally recommended a frozen bag of peas. I showed him GP and he loved the design.”

“Remote ✔
Gentlemen’s Parcel ✔
Junk Food ✔
Okay hunny, I’m ready to go…”
Medical & Scientific Studies
Supporting Cooling Therapy
and a Healthy Testicular Environment
to Improve Fertility, and the Health of the Child, Father, and Mother.
Further, your research with our list of studies from the medical and scientific community from over the past 50 years (in chronological order) supporting the effectiveness of testicular cooling and healthy testicular environment on sperm count, sperm quality, and testosterone.
Waites, G.M.H. and Voglmayr, J.K. (1963) The functional activity and control of the apocrine sweat glands of the scrotum of the ram. Aust. J. Agric. Res., 14, 839–851.
Rock, J. and Robinson, D. (1965) Effect of induced intrascrotal hyperthermia on testicular function in man. Am. J. Obstet. Gynecol., 93, 793–801.
National Center for Health Statistics, Rosenberg HM. Seasonal variation of births: United States, 1933–63. Vital and health statistics. Series 21. No. 9. Washington, D.C.: Government Printing Office, 1966. (PHS publication no. 1000.)
Robinson & Rock, 1967. Intrascrotal hyperthermia induced by scrotal insulation: effect on spermatogenesis. Journal of Obstetrics and Gynecology, 1967 Feb;29(2):217-23.
Robinson D, Rock J, Menkin MF. “Control of Human Spermatogenesis Intrascrotal Temperature.” JAMA. (1968); 204(4):290-297. doi:10.1001/jama.1968.03140170006002.
Fowler, D.G. (1969) The relationship between air temperature, scrotal surface area and testis temperature in rams. Aust. J. Exp. Agric. Anim. Husb., 9, 258–261.
Chowdhury, A. K., and E. Steinberger. "Early changes in the germinal epithelium of rat testes following exposure to heat." Journal of Reproduction and Fertility 22.2 (1970): 205-212
Zorgniotti, A.W. and MacLeod, J. (1973) Studies in temperature, human semen quality and varicocele. Fertil. Steril., 24, 854–863.
Zorgniotti AW, Seaflon A, Toth A: “Chronic scrotal hypothermia as a treatment for poor semen quality.” Lancet (1980), 315(8174):904-906.
Zorgniotti AW, Seaflon AI, Toth A: “Further clinical experience with testis hypothermia for infertility due to poor semen.” Urology (1982), 19(6):636-640.
Zorgniotti, A.W. (1982) Elevated scrotal temperature. II. Indirect testis and intrascrotal measurement for clinical and research use. Bull. N. Y. Acad. Med., 58, 541–544.
Brindley, G.S. (1982) Deep scrotal temperature and the effect on it of clothing, air temperature, activity, posture and paraplegia. Br. J. Urol. , 54, 49–55.
Mulcahy JJ: “Scrotal hypothermia and the infertile man.” The Journal of Urology (1984), 132:469-470.
Zorgniotti AW, Seaflon AI: “Scrotal hypothermia: new therapy for poor semen.” Urology (1984), 23(5):439-441.
Mieusset, R., Grandjean, H., Mansat, A. and Pontonnier, F. (1985) Inhibiting effect of artificial cryptorchidism on spermatogenesis. Fertil. Steril., 43, 589–574.
Mieusset et al, 1985. Inhibiting effect of artificial cryptorchidism on spermatogenesis. Journal of Fertility and Sterility, 1985 Apr;43(4):589-94.
Kurz, K.R. and Goldstein, M. (1986) Scrotal temperature reflects intratesticular temperature and is lowered by shaving. J. Urol., 135, 290–294.
Zorgniotti AW, Cohen MS, Seaflon I: “Chronic scrotal hypothermia: results in 90 infertile couples.” The Journal of Urology (1986), 135:944-947.
Lynch, R., et al. "Improved seminal characteristics in infertile men after a conservative treatment regimen based on the avoidance of testicular hyperthermia." Fertility and Sterility 46.3 (1986): 476-479.
Mieusset R, Bujan L, Mondinat C, et al. "Association of scrotal hyperthermia with impaired spermatogenesis in infertile men." Fertility and Sterility (1987); 48:1006–1011
Mieusset, R., Bujan, L., Mansat, A. et al. (1987) Effect of artificial cryptorchidism on sperm morphology. Fertil. Steril., 47, 150–155.
Mieusset, Roger, et al. "Hyperthermia and human spermatogenesis: enhancement of the inhibitory effect obtained by ‘artificial cryptorchidism’." International Journal of Andrology 10.4 (1987): 571-580.
Kaufman, D. G., and H. M. Nagler. "Specific nonsurgical therapy in male infertility." The Urologic Clinics of North America 14.3 (1987): 489-498.
Levine RJ, Bordson BL, Mathew RM, Brown MH, Stanley JM, Starr TB. Deterioration of semen quality during summer in New Orleans. Fertil Steril 1988; 49:900–7.
Laven, Joop SE, Michiel J. Haverkorn, and Rob SGM Bots. "Influence of occupation and living habits on semen quality in men (scrotal insulation and semen quality)." European Journal of Obstetrics & Gynecology and Reproductive Biology 29.2 (1988): 137-141.
Colter, G.H., Senger, P.L. and Bailey, D.R.C. (1988) Relationship of scrotal surface temperature measured by infrared thermography to subcutaneous and deep testicular temperature in the ram. J. Reprod. Fert., 84, 417–421.
Galil, K. A. A., and B. P. Setchell. "Effects of local heating of the testis on testicular blood flow and testosterone secretion in the rat." International Journal of Andrology 11.1 (1988): 73-85.
Chan, S. L. "Male Infertility: Diagnosis and Treatment." Canadian Family Physician 34 (1988): 1735.
Richard J. Levine, M.D., Ravi M. Mathew, M.S., C. Brandon Chenault, M.D., Michelle H. Brown, B.S.P.H., Mark E. Hurtt, Ph.D., Karin S. Bentley, Ph.D., Kathleen L. Mohr, B.S., and Peter K. Working, Ph.D. (July 5, 1990) Differences in the Quality of Semen in Outdoor Workers during Summer and Winter, N Engl J Med 1990;323:12-16 DOI: 10.1056/NEJM199007053230103 VOL. 323 NO. 1
Bedford, J. Michael. "Effects of elevated temperature on the epididymis and testis: experimental studies." “Temperature and environmental effects on the testis.” Springer US (1991). 19-32.
Waites, G.M.H. (1991) Thermoregulation of the scrotum and testis: studies in animals and significance for man. In Zorgniotti, A.W. (ed.), Temperature and Environmental Effects on the Testis. Plenum Press, New York, pp. 1–8.
Bonde, 1992. Semen quality in welders exposed to radiant heat. British Journal Independent Medicine, 1992, Jan., vol 49, pp 5-10.
Mieusset, R., Quintana-Casares, P., Sanchez-Partida, L.G. et al. (1992) Effects of heating the testes and epididymides of rams by scrotal insulation on fertility and embryonic mortality in ewes inseminated with frozen semen. J. Reprod. Fert. , 94, 337–343
Shafik, A. (1992) Testicular suspension as a method of male contraception: technique and results. Adv. Contrac. Deliv. Syst ., VII, 269–279.
Candas, V., Becmeur, F., Bothorel, B. and Hoft, A. (1993) Qualitative assessment of thermal and evaporative adjustments of human scrotal skin to heat stress. Int. J. Androl., 16, 137–142.
Lerchl A, Keck C, Spiteri-Grech J and Nieschlag E (1993) “Diurnal variations in scrotal temperature of normal men and patients with varicocele before and after treatment.” International Journal of Andrology 16, 195-200.
Mieusset, R. and Bujan, L. (1994). The potential of mild testicular heating as a safe, effective and reversible contraceptive method for men. Int. J. Androl. , 17, 186–191.
Mieusset R, Bujan L. Testicular heating and its possible contributions to male infertility: a review. International Journal of Andrology (1995); 18:169-184.
Figà-Talamanca I, Cini C, Varricchio GC, Dondero F, Gandini L, Lenzi A, Lombardo F, Angelucci L, Di Grezia R, Patacchioli FR. Effects of prolonged autovehicle driving on male reproduction function: a study among taxi drivers. Am J Ind Med. 1996 Dec;30(6):750-8. doi: 10.1002/(SICI)1097-0274(199612)30:6<750::AID-AJIM12>3.0.CO;2-1. PMID: 8914722.
Setchell, B.P. and Mieusset, R. (1996) Testis thermoregulation. In Hamamah, S. and Mieusset, R. (eds), Male Gametes Production and Quality. INSERM, Paris, pp. 65–88.
Thonneau, P., Ducot, B., Bujan, L. et al. (1996) Heat exposure as a hazard to male fertility. Lancet , 347, 204–205.
Bonde et al, 1998. Relation between semen quality and fertility: a population-based study of 430 first-pregnancy planners. The Lancet, 1998 Oct 10;352(9135):1172-7.
Thonneau et al, 1998. Occupational heat exposure and male fertility: a review. Journal of Human Reproduction, Volume 13, Issue 8, 1 August 1998, Pages 2122–2125.
Hjollund, Niels Henrik I., et al. "Diurnal scrotal skin temperature and semen quality." International Journal of Andrology 23.5 (2000): 309-318.
Louis Bujan, Myriam Daudin, Jean-Paul Charlet, Patrick Thonneau, Roger Mieusset, Increase in scrotal temperature in car drivers, Human Reproduction, Volume 15, Issue 6, 1 June 2000, Pages 1355–1357, https://doi.org/10.1093/humrep/15.6.1355
Jung A, Eberl M, Schill WB: “Improvement of semen quality by nocturnal scrotal cooling and moderate behavioral change to reduce genital heat stress in men with oligoasthenoteratozoospermia.” Reproduction (2001), 121:595-603.
Aitken RJ, Krausz C. Oxidative stress, DNA damage and the Y chromosome. Reproduction. 2001 Oct;122(4):497-506. doi: 10.1530/rep.0.1220497. PMID: 11570956.
Jung et al, 2001. Genital heat stress as a threat to male fertility. Andrologia, 33, 316-317.
Hjollund NHI, Storgaard L, Ernst E, Bonde JP and Olsen J (2002b) “Impact of diurnal scrotal temperature and semen quality.” Reprod Toxicol 16, 215-221.
Hjollund et al, 2002. The relation between daily activities and scrotal temperature. Reproductive Toxicology, May 2002, 16(3):209-214.
Power RE, Scanlon R, Kay EW, Creagh TA, Bouchier-Hayes DJ. “Long-term protective effects of hypothermia on reperfusion injury post-testicular torsion.” Scand J Urol Nephrol (2003); 37:456–460.
Sipos A, Rasmussen F, Harrison G, Tynelius P, Lewis G, Leon DA & Gunnell D. (2004) Paternal age and schizophrenia: a population based cohort study. BMJ 329, 1070.
Jung, A., et al. "Influence of the type of undertrousers and physical activity on scrotal temperature." Human Reproduction 20.4 (2005): 1022-1027.
Jung, A., Schill, W. -B., Schuppe, H. -C., ‘Improvement of semen quality by nocturnal scrotal cooling in oligozoospermic men with a history of testicular maldescent.’ International Journal of Andrology, vol. 28/2 (2005), pp. 93-98
Lewis SE, Aitken RJ. DNA damage to spermatozoa has impacts on fertilization and pregnancy. Cell Tissue Res. 2005 Oct;322(1):33-41. doi: 10.1007/s00441-005-1097-5. Epub 2005 Nov 3. PMID: 15912407.
Jung A, Schill WB, Schuppe HC: “Improvement of semen quality by nocturnal scrotal cooling in oligozoospermic men with a history of testicular maldescent.” International Journal of Andrology (2005), 28:92-98.
Borini, N. Tarozzi, D. Bizzaro, M.A. Bonu, L. Fava, C. Flamigni, G. Coticchio, Sperm DNA fragmentation: paternal effect on early post-implantation embryo development in ART, Human Reproduction, Volume 21, Issue 11, 1 November 2006, Pages 2876–2881
Reichenberg A, Gross R, Weiser M, Bresnahan M, Silverman J, Harlap S, Rabinowitz J, Shulman C, Malaspina D, Lubin G, Knobler HY, Davidson M & Susser E. (2006) Advancing paternal age and autism. Arch Gen Psychiatry 63, 1026–1032.
Mieusset, Roger, Bourras Bengoudifa, and Louis Bujan. "Effect of posture and clothing on scrotal temperature in fertile men." Journal of Andrology 28.1 (2007): 170-175.
Haj, M., et al. "Effect of external scrotal cooling on the viability of the testis with torsion in rats." European Surgical Research 39.3 (2007): 160-169.
Jung, A., and H‐C. Schuppe. "Influence of genital heat stress on semen quality in humans." Andrologia 39.6 (2007): 203-215.
Ivell, Richard. "Lifestyle impact and the biology of the human scrotum." Reprod Biol Endocrinol 5.15 (2007): 1477-1482.
Hammoud et al, 2008. Impact of male obesity on infertility: a critical review of the current literature. Journal of Fertility and Sterility, 2008 Oct;90(4):897-904.
Hansen, Peter J. "Effects of heat stress on mammalian reproduction." Philosophical Transactions of the Royal Society B: Biological Sciences 364.1534 (2009): 3341-3350.
Owen et al, 2010. Sedentary Behavior: Emerging Evidence for a New Health Risk. Mayo Clinic Proceedings, 2010 Dec; 85(12): 1138–1141.
Phillips and Tanphaichitr, 2010. Mechanisms of obesity-induced male infertility. Expert review Endocrinology & Metabolism. March 2010. 5(2):229-251.
Ferlin, Alberto, et al. "Heat shock protein and heat shock factor expression in sperm: relation to oligozoospermia and varicocele." The Journal of Urology 183.3 (2010): 1248-1252
Parviz Gharagozloo, R. John Aitken, The role of sperm oxidative stress in male infertility and the significance of oral antioxidant therapy, Human Reproduction, Volume 26, Issue 7, 1 July 2011, Pages 1628–1640
Sheynkin, Yefim, et al. "Protection from scrotal hyperthermia in laptop computer users." Fertility and Sterility 95.2 (2011): 647-651.
Menkveld et al, 2011. Measurement and significance of sperm morphology. Asian Journal of Andrology, 2011 Jan; 13(1): 59–68.
Vaziri MH, Sadighi Gilani MA, Kavousi A, Firoozeh M, Khani Jazani R, Vosough Taqi Dizaj A, Mohseni H, Bagery Lankarani N, Azizi M, Salman Yazdi R. The Relationship between Occupation and Semen Quality. Int J Fertil Steril. 2011 Jul;5(2):66-71. Epub 2011 Sep 23. PMID: 24963361; PMCID: PMC4059951.
Robinson L, Gallos ID, Conner SJ, Rajkhowa M, Miller D, Lewis S, Kirkman-Brown J, Coomarasamy A. The effect of sperm DNA fragmentation on miscarriage rates: a systematic review and meta-analysis. Hum Reprod. 2012 Oct;27(10):2908-17. doi: 10.1093/humrep/des261. Epub 2012 Jul 12. PMID: 22791753.
Sharpe, 2012. Sperm counts and fertility in men: a rocky road ahead. EMBO Reports, 2012 May; 13(5): 398–403.
Jenkins and Carrell, 2012. The sperm epigenome and potential implications for the developing embryo. Journal of Reproduction, Jun 2012.
Gannon et al, 2014 The Sperm Epigenome: Implications for the Embryo. Advances in Experimental Medicine and Biology, January 2014.
Garolla et al, 2015. Twenty-four-hour monitoring of scrotal temperature in obese men and men with a varicocele as a mirror of spermatogenic function. Journal of Human Reproduction, Volume 30, Issue 5, 1 May 2015, Pages 1006–1013.
Coughlan C, Clarke H, Cutting R, Saxton J, Waite S, Ledger W, Li T, Pacey AA. Sperm DNA fragmentation, recurrent implantation failure and recurrent miscarriage. Asian J Androl. 2015 Jul-Aug;17(4):681-5. doi: 10.4103/1008-682X.144946. PMID: 25814156; PMCID: PMC4492063.
Katib, 2015. Mechanisms linking obesity to male infertility. Central European Journal of Urology, 2015; 68(1): 79–85.
Rex AS, Aagaard J, Fedder J. DNA fragmentation in spermatozoa: a historical review. Andrology. 2017 Jul;5(4):622-630. doi: 10.1111/andr.12381. PMID: 28718529; PMCID: PMC5601286.
Anaissie J, DeLay KJ, Wang W, Hatzichristodoulou G, Hellstrom WJ. Testosterone deficiency in adults and corresponding treatment patterns across the globe. Transl Androl Urol. 2017 Apr;6(2):183-191. doi: 10.21037/tau.2016.11.16. PMID: 28540225; PMCID: PMC5422691.
Levine et al, 2017. Temporal trends in sperm count: a systematic review and meta-regression analysis. Human Reproduction Update, Volume 23, Issue 6, 1 November 2017, Pages 646–659.
Liu & Ding, 2017. Obesity, a serious etiologic factor for male subfertility in modern society. Journal of Reproduction, 2017 Oct;154(4):R123-R131.
Kahn & Brannigan, 2017. Obesity and male infertility. Current Opinion in Urology, 2017 Sep;27(5):441-445.
Braun et al, 2017. Fathers Matter: Why It's Time to Consider the Impact of Paternal Environmental Exposures on Children's Health. Current Epidemiological Reports. March 2017.
Rim Frikha, Taoufik Frikha, Nouha Bouayed, Tarek Rebai, Assessment of male factor involved in recurrent pregnancy loss: A preliminary study, Middle East Fertility Society Journal, Volume 23, Issue 3, 2018, Pages 238-240, ISSN 1110-5690
Mínguez-Alarcón L, Gaskins AJ, Chiu YH, Messerlian C, Williams PL, Ford JB, Souter I, Hauser R, Chavarro JE. Type of underwear worn and markers of testicular function among men attending a fertility center. Hum Reprod. 2018 Sep 1;33(9):1749-1756. doi: 10.1093/humrep/dey259. PMID: 30102388; PMCID: PMC6530653.
Rahman et al, 2018 Heat stress responses in spermatozoa: Mechanisms and consequences for cattle fertility. Theriogenology, June 2018.
Turner KA, Rambhatla A, Schon S, Agarwal A, Krawetz SA, Dupree JM, Avidor-Reiss T. Male Infertility is a Women's Health Issue-Research and Clinical Evaluation of Male Infertility Is Needed. Cells. 2020 Apr 16;9(4):990. doi: 10.3390/cells9040990. PMID: 32316195; PMCID: PMC7226946.
Christopher L R Barratt, Christopher J De Jonge, Richard A Anderson, Michael L Eisenberg, Nicolás Garrido, Satu Rautakallio Hokkanen, Csilla Krausz, Sarah Kimmins, Moira K O’Bryan, Allan A Pacey, Frank Tüttelmann, Joris A Veltman, A global approach to addressing the policy, research and social challenges of male reproductive health, Human Reproduction Open, Volume 2021, Issue 1, 2021, hoab009
Benidir T, Remondini T, Lau S, Jarvi KA. Evaluation of patient compliance with the use of scrotal cooling devices. F S Rep. 2021 Jun 30;2(3):289-295. doi: 10.1016/j.xfre.2021.06.007. PMID: 34553153; PMCID: PMC8441567.
Ferlin, A., Garolla, A., Ghezzi, M., Selice, R., Palego, P., Caretta, N., Di Mambro, A., Valente, U., De Rocco Ponce, M., Dipresa, S., Sartori, L., Plebani, M., & Foresta, C. (2021). Sperm Count and Hypogonadism as Markers of General Male Health. European Urology Focus, 7(1), 205-213. https://doi.org/10.1016/j.euf.2019.08.001
Malathi A, Iyer RP, Mohan R, Balakrishnan S. Impact of Seasonal Variations on Semen Parameters: A Retrospective Analysis of Data from Subjects Attending a Tertiary Care Fertility Centre. J Hum Reprod Sci. 2023 Apr-Jun;16(2):114-120. doi: 10.4103/jhrs.jhrs_20_23. Epub 2023 Jun 30. PMID: 37547085; PMCID: PMC10404019.
Zhao C, Sun L, Zhao P. Effects of sperm processing techniques on IVF pregnancy rates: a mini-review. Ther Adv Reprod Health. 2023 Jul 23;17:26334941231188656. doi: 10.1177/26334941231188656. PMID: 37497119; PMCID: PMC10366343.
Mínguez-Alarcón L, Williams PL, Souter I, Ford JB, Ghayda RA, Hauser R, Chavarro JE; Earth Study Team. Occupational factors and markers of testicular function among men attending a fertility center. Hum Reprod. 2023 Apr 3;38(4):529-536. doi: 10.1093/humrep/dead027. PMID: 36772979; PMCID: PMC10068265.
“All these years and I never knew my testicular and overall health were related. Good thing I went commando.”
Other lifestyle changes…
Along with Gentlemen’s Parcel and Cooling Therapy, we recommend improving other lifestyle factors that can contribute to low sperm count and quality such as diet, exercise, managing stress, avoiding tight clothing, not smoking, limiting alcohol, avoiding sexual lubricants, toxins, and overheating environments such as saunas, hot tubs, overly hot showers, and laptops on lap. Make sure to get enough vitamin C, vitamin D, B12, zinc, omega-3, and consider other supplements such as coenzyme Q10, maca root, ashwagandha, and fenugreek.
Diet is extremely important. Eat lots of antioxidant foods. For example, walnuts, ginger, blueberries, cranberries, strawberries, blackberries, raspberries, pomegranates, broccoli, spinach, carrots, potatoes, artichokes, cabbage, asparagus, avocados, beetroot, radish, lettuce, sweet potatoes, squash, pumpkin, collard greens, kale, tomatoes, garlic, onions, and extra virgin olive oil. Eat fatty fish and fresh meat, salmon, sardines, beef, and liver. Avoid eating processed meats, fried foods, soy, trans fats, and high-fat dairy products. Make sure to look out for BPA canned goods.
While exercise and movement are important- extreme training, cycling, and long-distance running can decrease sperm count and quality. Studies have shown that regular exercise including moderate weight-lifting, jogging, and aerobics can naturally boost fertility levels. If looking to conceive, don’t miss out on consistent sex during the 7-day window, 5 days before ovulation, and one day after. Get your heart pumping in more ways than one.
“We considered ourselves healthy but our sperm results were low and slow.”
Women are having fewer children
Global fertility rate (livebirths per woman)
Global Trends: Spermageddon! Male Fertility Crisis & Societal Impact.
Male infertility is a global issue that affects 17.5% of the world's adult population, or roughly 1 in 6 people. The prevalence of male infertility has increased from 1990 to 2019, with a growth rate of 76.9% compared to 1990. This increase is significant, especially when considering that the world population has only increased by 46% during the same period. The highest rates of male infertility are in Africa and Eastern Europe, with rates ranging from 2.5–12%. The global fertility rate has been declining since 1950, when it averaged five children per woman, and has reached 2.3 births per woman in 2021. This decline has occurred in all countries since 1950, and by 2021, more than half of all countries and territories had a fertility rate below the population replacement level of 2.1 births per woman. According to a 2020 study by The Lancet, the world's population will peak at 9.7 billion in 2064 and then decline to 8.8 billion by 2100. And then continue to decline. The study also predicts that by 2050, more than three-quarters of countries will not have high enough fertility rates to sustain population size over time. By 2100, this number will increase to 97% of countries. Over the past 70 years, there has been a significant decrease in birth rates across the nations. This trend is particularly evident in countries like China and South Korea, where birth rates have plummeted by over 80% since 1950. Other examples of countries high on the list include Japan, Italy, France, Ireland, Liberia, and the Republic of the Congo.
The new fertility forecasts underscore the enormous challenges to economic growth in many middle- and high-income countries with a dwindling workforce and the growing burden on health and social security systems of an aging population. According to the Lancet, dramatic declines in global fertility rates could reconfigure the global economy and the international balance of power. Some say that low birth rates in certain countries threaten "national security". Others warn that aging societies will represent a caretaking burden on society which will soon become unmanageable.
Pan American Health Organization, 2023. 1 in 6 people globally affected by infertility: PAHO/WHO.
Salib, V., 2023. A WHO Report Finds That 17.5% of People Experienced Infertility. Life Sciences Intelligence.
Huet, N., 2023. 'Global issue': 1 in 6 people worldwide affected by infertility, WHO report finds. Euronews.